Diabetic retinopathy affects over 93 million people globally. This eye condition, linked to diabetes, may result in vision loss and blindness if not addressed promptly. Understanding the risks and available treatments is vital for preserving eyesight.
What Is Diabetic Retinopathy?
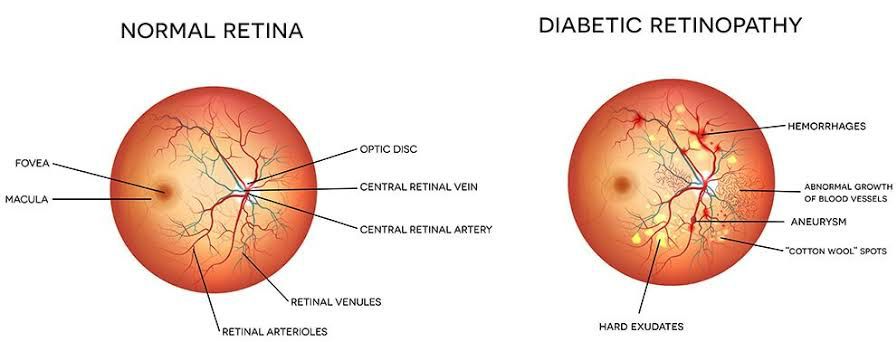
Diabetic retinopathy, commonly known as diabetic eye disease, is a disorder in which high blood sugar levels cause harm to the blood vessels in the retina.
The retina, a vital light-sensitive tissue at the back of the eye, turns light into electrical signals for the brain to interpret as pictures. When the retinal blood vessels are affected, it can impair vision and potentially lead to blindness.
Types of Diabetic Retinopathy
Diabetic retinopathy manifests in two primary forms, each with distinct characteristics and implications for vision health.
1. Non-Proliferative Diabetic Retinopathy (NPDR)
In the early stages of diabetic retinopathy, the blood vessels in the retina may weaken and leak fluid or blood. This can lead to swelling of the retina and vision problems.
2, Proliferative Diabetic Retinopathy (PDR)
As the condition progresses, new and abnormal blood vessels may grow on the retina’s surface. These fragile vessels are prone to leaking and may cause severe vision loss if not treated promptly.
Causes and Risk Factors
The primary cause of diabetic retinopathy is chronically high blood sugar levels, which may harm the small blood vessels in the retina over time. There are several other factors can increase the risk of developing this condition, including:
- Poorly controlled diabetes
- High blood pressure
- High cholesterol levels
- Pregnancy (gestational diabetes)
- Smoking
- Prolonged diabetes duration
Symptoms of Diabetic Retinopathy
In the early stages of diabetic retinopathy, individuals may not experience any noticeable symptoms. As the condition progresses, the following symptoms may become apparent:
- Blurred or distorted vision
- Floaters, or dark spots in the field of vision
- Difficulty seeing at night
- Changes in colour perception
- Vision loss
Diagnosing Diabetic Retinopathy
Regular eye exams are critical for detecting and managing diabetic retinopathy early. The ophthalmologist will dilate the pupils during an eye exam to check the retina and optic nerve for signs of damage.
Other diagnostic test options, such as optical coherence tomography (OCT) and fluorescein angiography, may be used to determine the degree of retinal damage.
Treatment Options for Diabetic Retinopathy
Several effective treatment options are available to manage diabetic retinopathy and prevent vision loss. Here are the key approaches to address this severe eye condition.
1. Laser Photocoagulation
This treatment involves using a laser to seal off leaking blood vessels and prevent them from causing further damage to the retina. Laser photocoagulation is effective for managing proliferative diabetic retinopathy.
2. Anti-VEGF Injections
Anti-VEGF (vascular endothelial growth factor) injections minimize the growth of unusual blood vessels in the retina and reduce swelling. These injections are commonly used to treat macular oedema, a complication of diabetic retinopathy affecting central vision.
3. Vitrectomy
In advanced cases of PDR with significant bleeding into the vitreous gel, a vitrectomy may be necessary to remove the blood and scar tissue and restore vision.
4. Steroid Implants
Tiny steroid implants can be placed in the eye to reduce inflammation caused by diabetic retinopathy and improve visual outcomes.
Preventing Diabetic Retinopathy
Preventing diabetic retinopathy starts with managing diabetes effectively. Here are some essential tips for reducing the risk of developing this eye condition:
-
- Regular medical check-ups
- Healthy lifestyle
- Avoiding smoking
- Regular eye exams