Diabetic retinopathy is a chronic diabetic complication that affects the light-sensitive tissue of the eye’s retina. This is caused by damage to the blood vessels.
Diabetic retinopathy can be tricky to deal with as it shows little to no symptoms initially, but in the later stages, the retina starts to bleed. At this point, the person diagnosed will see dark spots or streaks, and if the diabetes isn’t brought under control it can cause vision loss and blindness. Physical activity and healthy eating habits can help one prevent long-term vision impairment.
It is no surprise that diabetes is the biggest precursor to diabetic retinopathy, with those afflicted always in danger of falling victim, with the risk ever-increasing with time.
Let’s go over the causes in a detailed way:
Table of Contents
Diabetic Retinopathy Causes
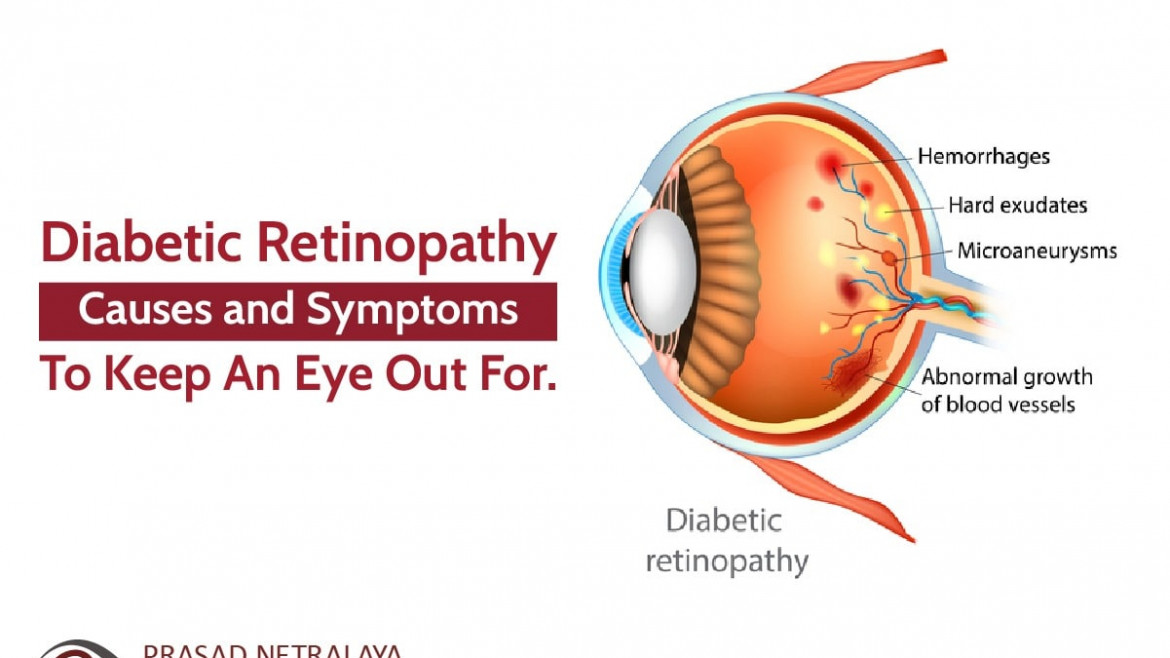
The presence of high blood sugar due to diabetes and duration of the diabetes are the chief cause of diabetic retinopathy. The damage to the retina starts when blood supply to the retina is gradually blocked and new blood vessels start to develop. This causes the retina to bleed. These blocked blood vessels are only partially replaced by new ones by the eyes, which may not be as effective.
There are two types of diabetic retinopathy:
1. Non-Proliferative Diabetic Retinopathy (NPDR)
Initial stages of diabetic retinopathy. Gradual blocking of vessels will lead to development of many hemorrhages in retina and fluid and lipid exudation in retina. As more blood vessels become blocked, NPDR develops from mild to severe. Sometimes, this can lead to the buildup of fluid, often known as diabetic macular oedema, in the macula of the retina which can severely affect one’s vision.
2. Proliferative or Advanced Diabetic Retinopathy
The damaged blood vessels in the retina close off leading to the development of abnormal blood vessels. These new blood vessels are quite fragile and cause the blood to leak into the vitreous, i.e. the clear gel between the lens and the retina leading to vitreous hemorrage. Eventually, the retina detaches from the back of the eye leading to tractional retinal detachment. This more severe type can lead to glaucoma or the damage of the optic nerve which carries images from the eye to the brain.
Diabetic Retinopathy Symptoms
As discussed earlier, it is hard to observe any symptoms in the earlier stages, but the longer one suffers from diabetes, the more diabetic retinopathy develops as the symptoms begin to show. One can experience spotty, blurry, or hazy eye vision. Sometimes, spots or dark strings floating in your vision make it difficult to perceive colours. In severe conditions, it can lead to vision loss but it can be prevented if diabetes is managed carefully.
Diabetic Retinopathy Treatment:
While one cannot always prevent diabetic retinopathy, with good management of blood sugar, blood pressure, and regular eye tests, they can prevent severe vision loss or impairment.
- Control your diet with healthy eating followed by taking insulin or diabetic medications regularly as directed.
- Constantly monitor your blood sugar level and consult your doctor if any fluctuations are observed.
- Be physically active. Walk for at least two hours a week or commit to similar moderate aerobic activities.
- Ask your doctor for a glycosylated haemoglobin test, or A1C test, which reflects your average blood sugar levels. Commonly, the A1C goal must be under 7%.
However, these are only for mild cases. Advanced cases may require laser treatment, eye injections or diabetic retinopathy surgery. Get the best consultations at Prasad Netralaya, where our expert and experienced ophthalmologists and surgeons ensure all-around care for your eyes. To know more, call us at +91 9513596565 to book an appointment. You can also book a teleconsultation here.
Dr. Vikram Jain, M.S. had his medical training (MBBS) from Kasturba Medical College, Mangalore, India. He did his master’s in Ophthalmic surgery from Kasturba Medical College, Manipal. He currently manages the Glaucoma department of Prasad Netralaya hospital.